The use of this dye with green light generates reactive oxygen species, which can be toxic to infectious pathogens, and also results in decreased corneal melting.
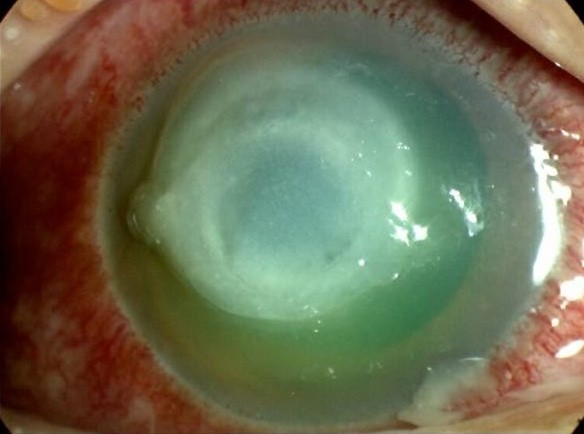
Acanthamoeba keratitis in a contact lens-wearer, presenting with a ring infiltrate and corneal melting.
Infectious keratitis is a corneal infection that can progress rapidly and lead to visual deterioration if not managed promptly and adequately. The current standard of care involves the frequent administration of topical antibiotics, sometimes in combination with periocular or systemic drugs as well. In more advanced cases, a therapeutic penetrating keratoplasty (TPK) may have to be performed. Recently, photo-activated chromophore corneal collagen crosslinking (PACK-CXL), in which riboflavin was irradiated with ultraviolet-A (UV-A) light, was shown to be an effective technique for the treatment of progressive presumed infectious keratitis that may have antimicrobial resistant microbes.
Rose Bengal photodynamic antimicrobial therapy (RB-PDAT) has also been shown to be efficient in vitro, as a treatment for keratitis with fungi and methicillin resistant Staphylococcus aureus (MRSA) as the offending agents. With this strategy, rose Bengal is excited with a green light (λ: 500-550 nm) to generate reactive oxygen species (ROS) that can be toxic to bacterial, viruses, fungi and protozoa. Previous in vivo and ex vivo experiments have shown that this treatment has no significant adverse events on keratocytes or on deeper tissues of the eye.
This study was a retrospective chart review of all the patients with presumed infectious keratitis who underwent RB-PDAT at an academic enter throughout 27 months. RB-DAT was performed because these patients were considered resistant to treatment, having already received the standard medical therapy for 2 weeks and showing no clinical improvement.
A total of 18 patients (19 eyes) were analyzed throughout the follow-up period. A microbiologic diagnosis was confirmed in 17 patients, with the most common infecting species: Acanthamoeba spp., Curvularia spp., and Pseudomonas aeruginosa.
RB-PDAT was considered successful in 13 patients, as there was control of the infection without the need for TPK. The time for resolution in these patients, from the first RB-PDT session, was 46.9 ± 26.4 days. No organisms were identified on pathology or microbiology from the hot tissue removed after later penetrating keratoplasties (PKP) and deep anterior lamellar keratoplasties (DALK), which occurred in 7 and 2 patients, respectively. The best corrected visual acuity (BCVA) also improved 1.92 ± 0/8 LogMAR (p<0.01) from presentation to one-year follow-up.
As for the other 5 patients, corneal perforation occurred after treatment with RB-PDAT. Even after TPK, 3 grafts had corneal edema and neovascularization, with one having to undergo enucleation. Only one graft remained clear after TPK. Demographics and the clinical characteristics of the infection, including, depth, epithelial size defect, the area of the infiltrate, and the period of prior medical treatment, did not predict the risk of RB-PDAT failure. Interestingly, non-contact lens wearers had a significantly higher risk of RB-PDAT failure versus contact lens wearers.
This pilot clinical study showed the effectiveness of the RB-PDAT treatment in infectious keratitis. The authors postulated that even if rose Bengal interacts strongly with collagen and is limited to a penetration of 100 μm into the stroma, photochemical crosslinking halted corneal melting, preventing the worsening of the infection and allowing topical antimicrobials to work.
Hence, RB-PDAT has potential as an adjunct when used for patients with infectious keratitis that are not responding to treatment, in an effort to avoid TPK and optimize for the best visual outcomes.
Naranjo, A., Arboleda, A., Martinez, J., Durkee, H., Aguilar, M., & Relhan, N. et al. (2019). Rose Bengal Photodynamic Antimicrobial Therapy (RB-PDAT) for Patients with Progressive Infectious Keratitis: A Pilot Clinical Study. American Journal of Ophthalmology. doi: 10.1016/j.ajo.2019.08.027