Better designed studies will facilitate a greater understanding of the physiology and pathology of IOP changes, making glaucoma treatments more reliable.
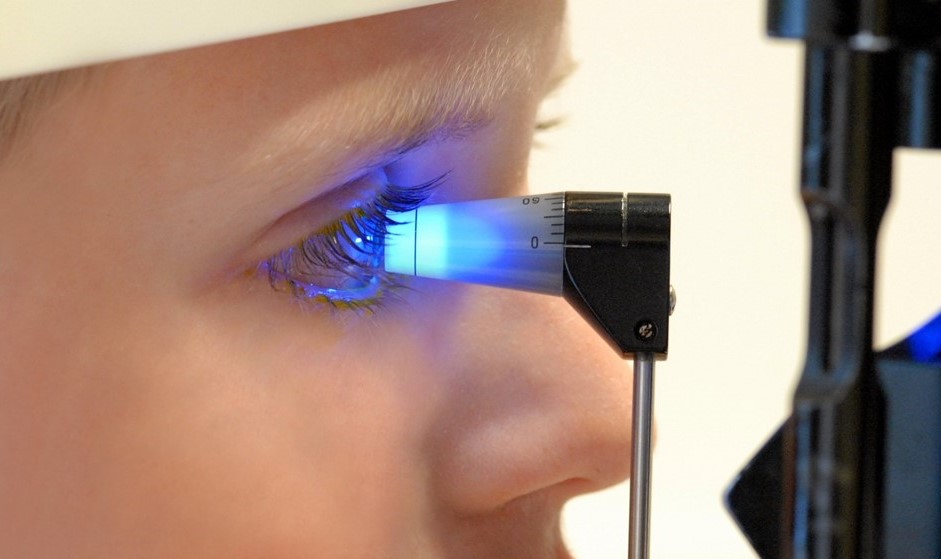
In the ophthalmology office, the most common and reliable method of measuring intraocular pressure is applanation tonometry.
Glaucoma is the most common cause of reversible blindness worldwide. One of the clinical presentations is increased intraocular pressure (IOP), and lowering the IOP via medical, laser, or surgicaal interventions is presently the only known method to mitigate disease progression.
However, the IOP has been documented to fluctuate throughout the day, and single in-office measurements during visits to the ophthalmologist’s office only give limited information. Previous studies have shown that the peak IOP has often been measured at night. Clinical research that has been done on glaucoma should account for circadian differences in the IOP to better analyze the effect of the treatments being tested.
This study looked at several previous researches conducted that utilized a 24-hour IOP monitoring system, after which recommendations were made.
- Obtaining multiple IOP pressure measurements even outside the office, including when the patients are in their habitual position at night. This will ensure that the measurement will align with the body’s circadian rhythm and positioning.
- However, nocturnal monitoring may not always be necessary, as it has been previously shown that multiple daytime measurements are on par with predicting disease progression, as with 24-hour monitoring.
- Variability in 24-hour monitoring can be due to differences in patient characteristics (race, ethnicity, age). Hence, patient populations must be properly characterized when stating IOP measurements.
- IOP measurements must also be done using calibrated tools. The same instrument must be used for all measurements. It is also best to use measurement techniques that minimize disturbances to the patient’s natural state.
- Long-term fluctuations in IOP must be differentiated from short-term fluctuations by factoring in diurnal variability, measurement error, and other factors.
Mansouri, K., Tanna, A., De Moraes, C., Camp, A., & Weinreb, R. (2019). Review of the measurement and management of 24-hour intraocular pressure in patients with glaucoma. Survey of Ophthalmology. doi: 10.1016/j.survophthal.2019.09.004